
Team members
Kenza Benmansour, Lana Kang, Kiana Ngai, Malek Medkour, Naya Wardeh, Houwen Yao
Project summary
MYBO: A dedicated AI companion for functional neurological disorder (FND) patients, designed to prevent stressful flare-ups, to inform and to help them regain agency.
Keywords
Waitlist companion, Nervous system dysregulation, Heart-rate variability (HRV), Functional conditions, Functional neurological disorders (FND)
Inspiration
Why We Built MYBO: A Nervous System Companion for stigmatized conditions
In healthcare, there’s a particular kind of pain that often goes untold: the pain of not being believed. For millions living with functional conditions, the symptoms are real, but the support is not. These are disorders where the body’s systems stop working properly despite normal test results, often driven by nervous system dysregulation, which include conditions like Functional Neurological Disorder (FND), Irritable Bowel Syndrome (IBS), chronic fatigue, and chronic pain. Patients are met with stigma, told it’s “just stress,” and sent home with no answers and no tools. This kind of pain is one that two of our team members have faced themselves, living with FND and with chronic pain. The value of lived experience always serves as an unmatched motivation to solve real problems that deserve more attention.
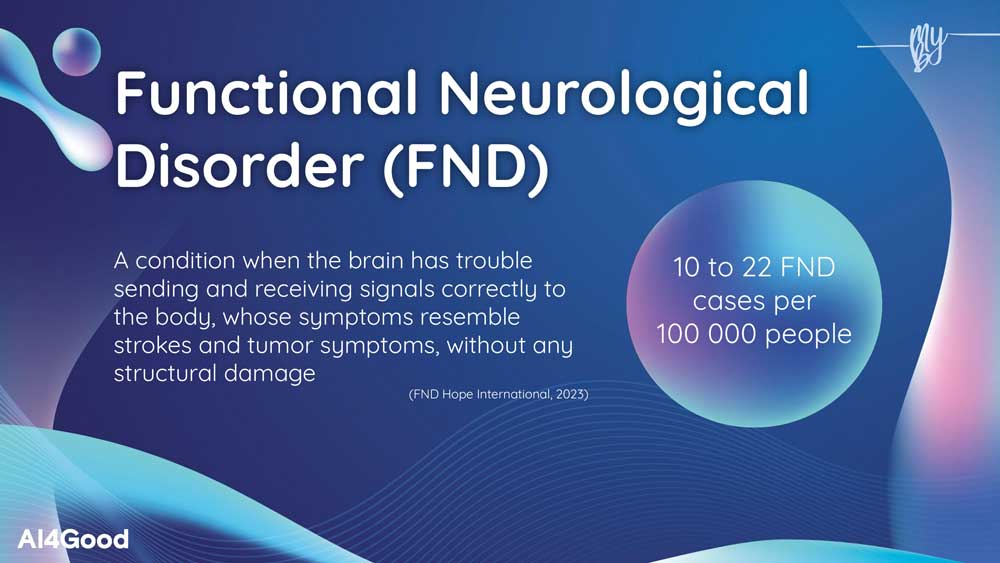
The problem we’re addressing is urgent and deeply human. Functional disorders involve real disruptions in how the nervous system processes signals, but because they don’t show up on standard scans, they are misunderstood and mismanaged. Patients often spend years on waitlists for care after diagnosis, cycle through specialists, or are told it’s “psychological”, with no guidance on what to do in the meantime.
Thus, we wanted to build something that could step into that gap. A companion, not a cure. A way to make sense of the chaos happening inside the body and gently support people through it. We imagined this solution; a mobile app that uses biofeedback and AI to help users regulate their nervous system, track their symptoms and have access to educational tools on their condition.
At its core, MYBO seeks to combine heart rate variability (HRV), a well-established, non-invasive biomarker of autonomic nervous system activity, with simple check-ins about mood, symptoms, and context. HRV can act as an indicator of heightened stress, emotional overload, or the early onset of dysregulation, all of which are common in functional disorders. Using this data, our AI models can detect patterns and forecast when a user may be approaching a state of nervous system stress. The app then offers gentle, personalized regulation tools, such as breathing exercises, somatic grounding, or education about what’s happening in the body.
However, MYBO is still not a diagnostic tool. It is not a replacement for therapy or medical care, but it is a bridge for the people who are waiting, dismissed, or simply overwhelmed. It helps users build a better mind-body connection and understand their own nervous system rhythms over time. The science is there: research shows that improving stress regulation and HRV through practices like biofeedback and breath regulation can significantly improve symptoms across many functional and stress-related conditions. But this kind of support rarely reaches those who need it most, especially in a form that’s personalized, compassionate, and grounded in real lived experience.
List of technologies
Machine Learning and Data Processing:
Keywords: Pandas, Sklearn, Seaborn, Matplotlib, RandomForestClassifier, LogisticRegression, KaggleHub, Google Colab.
We first explored several datasets from Kaggle, OpenNeuro, and PhysioNet. After filtering for datasets that collected fine-grained HRV data with stress labels, we chose SWELL-KW as our main dataset. Since we found this on Kaggle, we could directly load the data using KaggleHub. We split the data into test-val-train subsets to validate and generalize our work, and set the random seed for reproducibility. We used Python packages like Numpy, Pandas, Seaborn, and Matplotlib to first summarize our data with tables and then visualize the correlations between the features to note any redundancy or noise.
To build the actual ML models, we used Scikit-learn’s Ensemble (Random Forest (RF) Classifier) and LinearModel (Logistic Regression) models, then tested their performance using Scikit-learn’s Metrics module. These models were chosen mainly for their accessibility and interpretability, as we were able to extract the top features with the RF model, for example.
To incorporate the model with the application, we exported the models using Pickle. We further used Apple Watch and Apple HealthKit to obtain HRV readings from one of our team members, and used it to check compatibility with the model and the MYBO mobile app.
App Development (Frontend, Backend, Deployment):
Keywords: Python, React Native, Expo Go, FastAPI, TypeScript, Figma, GitHub.
We began the design of the frontend in Miro, which allowed us to create graphs to outline the flow and functionality of the app, drawing from existing app designs and flowcharts for reference. See our flowchart below.
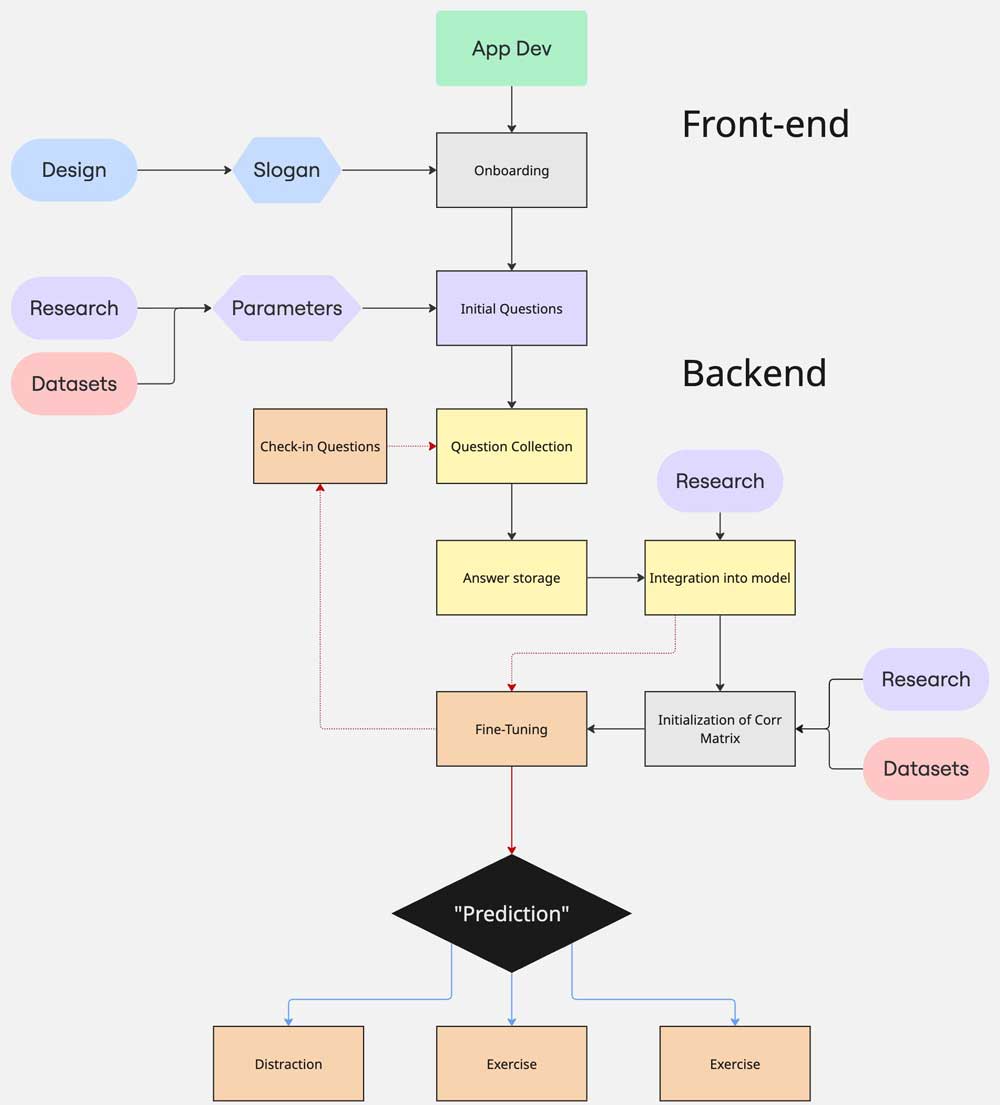
We drafted the UI design of the app in Figma with the goal of using soothing colors and gradients in reflection of our app’s mission. The frontend of the app was coded in TypeScript with React Native, and the backend was coded in Python with FastAPI. This setup allowed us to run the ML model in the backend and communicate the result back to the frontend.
We compiled the codebase using the Expo framework, which allowed us to quickly debug our changes locally with the Expo Go mobile app without the need to build it every time. It helped us preview how the app would be displayed on our phones, and we used it during Demo Day as well.
The aforementioned steps involved a lot of back-and-forth, as we would revise our app design, UI and backend as we started implementing them.
Project development
What does it do?
MYBO guides a user with functional neurological disorder (FND) through an interactive journey to reconnect with their body and regain agency over their symptoms. Ultimately, the goal is for users to connect a wearable (ie. Apple Watch, Fitbit or Garmin) to allow access to constant heart rate variability (HRV) measurements. As such, when the ML model detects any signs of nervous system dysregulation, users would receive reminders for a regulation exercise.


What is HRV and how does it relate to stress measurements?
Heart rate variability (HRV) is a measurement of the difference in time interval between heart beats. Variation is normal despite common belief that heart rate should be consistent (HeartMath, 2023). The variation is a sign of healthy exchange between the parasympathetic and sympathetic branches of your autonomic nervous system (HeartMath, 2023; Kim et al., 2018). This suggests that the larger the variation, the better your system can regulate stress. Lower variations are typically associated with flare-ups in functional conditions (Kim et al, 2018).
How does it work?
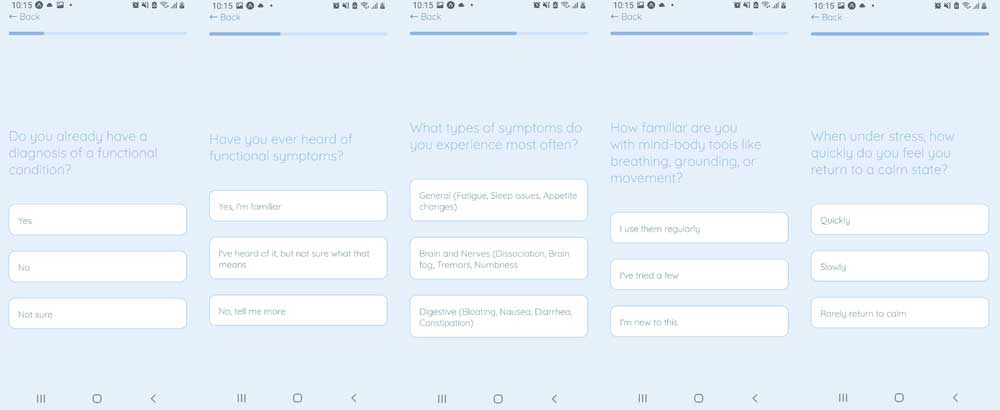
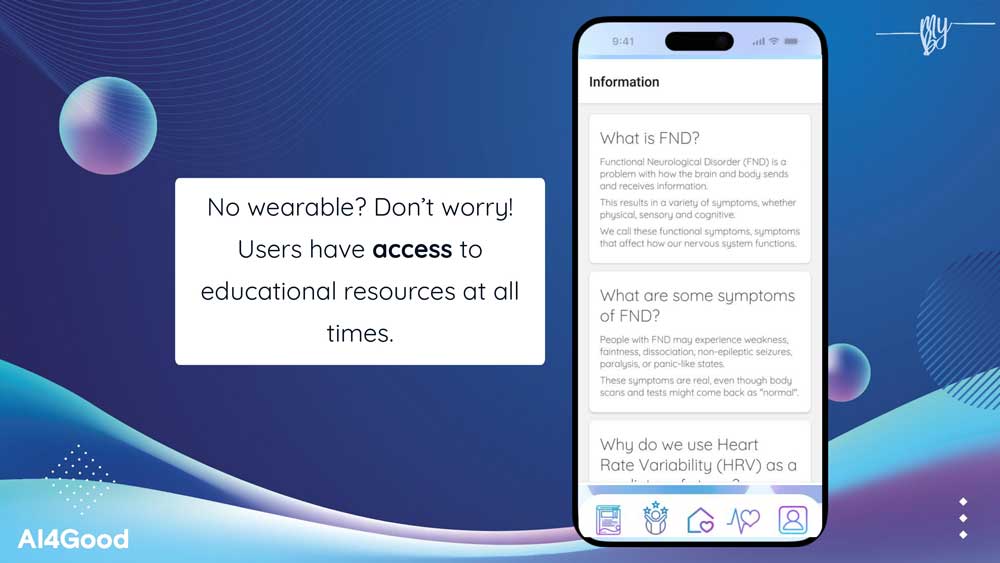
We first offer the user an onboarding process, where they indicate their diagnosis and their familiarity with regulation techniques. Then, based on available HRV data, our ML model predicts whether an example user would exhibit signs of nervous system dysregulation. At all times, users have access to a library of different regulation techniques recommended for them. We built this library based on clinician-approved exercises commonly used to restore the mind-body connection for FND patients. Moreover, users would be able to find an education section that includes information about their diagnosis along with a directory of trusted resources. We verified both our library of tools and education section with Dr. David Benrimoh, a Montreal-based neuropsychiatrist and researcher working with FND and AI.

Why is this a good machine learning use case?
It is unknown to the FND patient community when and how they will experience dysregulation during their day. For some it is chronic, and for others it is intermittent, but it is hard for them to monitor any indicators and make predictions, and prepare themselves accordingly.
Our system uses AI to identify patterns in HRV and self-reported symptoms to predict moments of heightened nervous system dysregulation and stress. It then gently suggests personalized, evidence-based mind-body regulation techniques, such as breathwork, grounding, or movement, to help soothe the nervous system and reduce symptom escalation without alarming the user. Hence, with Machine Learning, patients can understand their trends with more ease and comfort.
What dataset(s) did you use?
To train our machine learning model to predict stress based on heart rate variability (HRV) measurements, we used the multimodal SWELL knowledge work (SWELL-KW) dataset (Biometrics for Stress Monitoring). This dataset, collected for research on stress and user modeling at Radboud University in the Netherlands, consists of the data of 25 participants doing typical office work, while undergoing three different stress conditions (no stress, time pressure and interruption). This dataset recorded both biophysical data and subjective experience throughout multiple time points, including ECG signal (electrocardiogram of the heart), skin conductance (electrical activity of sweat glands, proxy for stress/arousal), emotion, and perceived stress. These features were perfect to train a simple logistic regression model, which attained a test accuracy of 82.51% for 70/30 train-test split.
Moreover, one of our team members recorded her HRV measurements throughout the past two months using her Apple Watch and the Health app. We verified that the necessary HRV data (BPM and SDNN) could be extracted, was compatible with the input features that the AI model requires, and was hence used for the demo.
Impact/Innovation
Who are our competitors and how are they addressing the issue?
We compiled a list of competitors or related apps in terms of design or mission:
- Finch: self-care app
- Flo: Period tracking app
- Calm: breathing and meditation app
- Headspace: breathing and meditation app
- Nerva: IBS management app
- VISIBLE: for illness tracking, using HRV
We also had a general look at the wellness app space available on mobile. The competitors we dove most deeply into were Nerva (primarily for its onboarding process) and VISIBLE (as it had the closest mission to ours).
Nerva’s onboarding was streamlined and user-friendly, with questions framed to be for “checking if our program is a good fit for you.” We noted some features like the ability to go back, short elaborations placed on new lines, a progress bar, and the occasional “I’m not sure” or “Other” options. We also paid attention to the types of questions they asked, such as existing diagnosis, treatment history, and personal goals. Nerva also integrates validating phrasing and educational intermissions between questions, though the explanations don’t actually adapt to your answers or self-reported expertise on the topics. The process ends with the app establishing credibility by referencing partnerships with doctors.
Looking at VISIBLE was also very helpful, as the app itself aligns closely with our mission. It seemed to include a lot of the features we were aiming to implement and had an established userbase, which encouraged us to reflect more deeply on what we wanted our app to do and how we could set it apart from similar services.
Beyond the design considerations, we also noticed that some of the apps in the wellness space come with significant costs, which could prevent some users from getting help. Additionally, while reviewing terms and policies, we noticed that some apps included fine print around data privacy that could be concerning or unclear for users. This reinforced our commitment to prioritize transparency and accessibility in our own app and business model moving forward.
What potential impact could your project have on its intended audience or field?
Our primary audience, individuals diagnosed with FND, is a population often left without adequate support or understanding after diagnosis. Our app offers real-time physiological feedback and personalized interventions, and by that our potential impact on our audience aims to:
help users stabilize their symptoms through nervous system regulation tools (e.g. HRV-based breathing or grounding), accompany them throughout their healing journey, supporting but not replacing their ongoing therapy, educate and empower users who have a diagnosis but lack clear guidance on how to manage their condition day to day, bridge the care gap for those waiting months for a specialist appointment.
In the long term, we aim to broaden access to individuals experiencing related psychosomatic disorders, such as chronic pain, dissociation and fibromyalgia, offering each user a personalized and scientifically grounded companion for mind-body recovery.
As Angela Glover Blackwell, an American attorney, civil rights advocate, and author, says in the Stanford Social Innovation Review: “Laws and programs designed to benefit vulnerable groups, such as the disabled or the poor, often end up benefiting everyone”. At MYBO, we know that our efforts to help individuals diagnosed with FND will end up helping the rest of the population.
What are the socio-technical ethical implications of this project on society, and how did you address ethical concerns?
This project carries several important socio-technical and ethical implications for society, particularly for those living with Functional Neurological Disorders (FND), as well as stakeholders like medical professionals, neuropsychiatrists, and patients’ families and support networks.
Stakeholder Involvement and Ethical Design
We addressed ethical concerns by including stakeholders throughout the design and development process. We consulted Dr. David Benrimoh, a neuropsychiatrist with expertise in FND and AI, to understand clinical perspectives and to ensure that MYBO could complement, rather than conflict with, existing medical practices. His feedback helped validate the concept and refine our educational resources and tools library. We also engaged directly with the FND community through a Google Form survey, which allowed us to better align the app with users’ values, needs, and concerns.
Addressing Data Bias and Fairness
We carefully considered the potential for bias in our training dataset, SWELL-KW, which was composed entirely of data from healthy participants. Since FND patients may have different HRV (heart rate variability) baselines, this could introduce model inaccuracies or unfair assumptions (Kim et al., 2018). To mitigate this, we propose collecting anonymized user data through an opt-in, informed consent process, ensuring users retain full control over their data and can opt out at any time. Our long-term goal is to develop personalized models tailored to each user’s unique physiological patterns, minimizing generalization bias.
Accessibility and Inclusivity
We also considered accessibility to ensure MYBO can be useful to a broad range of users. While the app encourages integration with wearable devices for HRV tracking, all users—regardless of device ownership—can freely access the full library of educational resources and self-regulation exercises. By prioritizing the educational component, we aim to empower users with tools for emotional regulation, even without physiological data inputs. The app’s design includes inclusive prompts such as, "Do you have a wearable device? Y/N" to adapt the experience accordingly.
What potential harms could arise from your solution?
While our goal is to create a positive impact, we acknowledge that potential harms may arise from our solution. Using what we learned in our ethical AI consultation with Rose Landry, we considered who our stakeholders are and brainstormed some of their core values. Next, we identified possible conflicts between their core values. For example, while users may desire highly personalized experiences—which require collecting and training on sensitive data—they also strongly value data privacy and control. This tension is central to many digital health solutions.
Data Privacy vs. Personalization
Personalization often requires collecting detailed physiological and behavioral data. To mitigate privacy risks, we implement opt-in data collection with clear, informed consent and the option to opt out at any time. Our goal is to strike a balance between utility and user autonomy, ensuring transparency in how data is used and stored.
Emotional and Psychological Risk
We recognize that any emotional regulation tool could have unintended effects. To minimize potential harm, MYBO only recommends gentle, evidence-informed regulation techniques. These are designed to support, not disrupt, a user's emotional state.
Risk of Over-Reliance
We intentionally designed MYBO with the long-term goal of reducing user dependency on the app. The app encourages skill-building and autonomy, so users eventually feel empowered to regulate independently. We consider this gradual reduction of reliance a key ethical strength of the solution.
Misuse or Misinterpretation
As with many health-related technologies, there’s a risk that users might misunderstand the app’s purpose or use it in place of professional care. To mitigate this, we include a clear disclaimer stating that MYBO is not a substitute for medical or psychiatric advice. However, we recognize this boundary can be blurred, so our messaging and educational content are carefully framed to reinforce this distinction.
Challenges
An initial challenge we faced was translating our ideas into a concrete, feasible product. Defining the scope of the project was difficult, as we had ambitious aspirations. We overcame this by brainstorming and listing everything we had in mind, then prioritizing ideas based on what was realistic to accomplish by Demo Day versus what could be developed in the long term. Sometimes, we would realize our scope was still too broad, which made the work feel overwhelming. We addressed this by finally narrowing our focus — starting with a minimal viable product and expanding only if we had enough time and resources.
Another challenge was maintaining motivation throughout the project timeline. Like many long-term efforts, we hit occasional slumps in energy and drive. To push through, our TA, Prakhar, helped us set small, achievable milestones to help us track progress and celebrate small wins. Focusing on the next step, rather than the entire final product, helped make the project feel more manageable. It also helped that we worked tightly as a team and talked to each other and other mentors to support each other through our individual and collective slumps.
What we learned and accomplished
We learned a lot throughout the AI4Good program — both technically and personally.
From the program itself, we learned the foundations of machine learning and gained some valuable and practical insight into the ethical implications of AI and how to use it responsibly for social good. The delivery was engaging and diverse, with experienced speakers covering topics from climate change and mental health, to AI policy and the perspectives of Indigenous communities. As the weeks went on, we learned (and re-learned) to question our assumptions and push the boundaries of our ideas. Through our weekly Friday projects, we practiced working under pressure, learning to manage our time and tasks effectively, and making the most of team collaboration. We also discovered the importance of seeking help when needed—whether from mentors, TAs, or peers—and the value of asking the right questions. Finally, we practiced presenting our ideas and building an engaging and persuasive pitch, while gaining a deeper understanding of what it takes to build a product from the ground up.
From developing our project, we learned how important communication and conflict resolution are to a team’s success. As cliché as it may sound, “teamwork makes the dream work” really held true for us. Challenges were inevitable, but we learned that the foundation for resolving them is honest, respectful communication. Being vulnerable and expressing concerns can be difficult, but it’s necessary for building trust. One of the biggest personal lessons we took away is that strong team dynamics require intentional effort. Trust is like a seed that needs to be nurtured over time. As we move forward in our individual journeys, we hope to continue cultivating that mindset in all future collaborations.
What’s next for the project
For the future, the AI we envision will learn from each user’s unique baseline, tailoring its responses not just to general patterns, but to each person’s physiology, symptom history, and context over time. This means smarter, more precise support that respects the complexity of real bodies and real lives.
Right now, we’re focusing on building a strong, ethical foundation. But we know that to reach our full potential, we need to integrate with wearable technology. That means working toward real-time HRV detection, a critical step to making MYBO more responsive, predictive, and clinically useful. At the moment, the app can't yet read HRV data live from a wearable, but this is a major technical milestone we’re actively planning for. The next phase of development will include connecting with devices like smartwatches.
We also recognize that health is shaped by identity and lived experience. Due to current data limitations, we were not able to train our model using a demographically diverse dataset. But we’re committed to improving this in the future, prioritizing inclusion across age, gender, and ethnicity, all of which can impact both diagnosis and symptom presentation.
We’re also expanding beyond FND. Conditions like chronic pain, IBS, PMDD, fibromyalgia, Long COVID, and other under-researched, waitlisted disorders where stress regulation and the nervous system often play a role are part of our vision.
Moving forward, our next step is to join an incubator or health innovation program where we can access mentorship, technical support, and clinical partnerships. With the right resources, we hope to refine our biofeedback integration, strengthen our AI models, and co-design with users and clinicians alike.
MYBO started as a deeply personal project, but what it’s growing into is a collective mission: to give people with functional conditions the support they’ve long been denied and the tools to reclaim their nervous system.
Acknowledgements & References
Acknowledgements:
Special thank you to everyone who helped guide and support us throughout the project weeks:
- Prakhar Ganesh and Jeremy Pinto for their wonderful mentorship;
- Dr. David Benrimoh for clinical advisorship;
- Rose Landry for responsible AI feedback;
- Aaron Labbé and Darius Valevicius for their consultancy on tech and neuroscience;
- Yohan Alphonse for website design;
- Karla Felix Navarro for pitch feedback;
- Jennifer Addison, Juliana Virani, and Dr. Yosra Kazemi for their amazing support
And everyone from: AI4GOOD LAB, MILA, CIFAR, Google Deepmind, Manulife, Vector Institute, Amii
References:
- Biometrics for Stress Monitoring [Dataset]. Kaggle. Retrieved April 27, 2023, from https://www.kaggle.com/datasets/qiriro/stress
- HeartMath (2023). The Science of HeartMath. https://www.heartmath.com/science/#
- Kim, H-G, Cheon, E-J, Bai, D-S, Lee, Y. H., & Koo, B. H. (2018). Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig, 15(3), 235-245. doi: 10.30773/pi.2017.08.17
- Nkurikiyeyezu, K., Yokokubo, A., & Lopez, G. (2020). The Effect of Person-Specific Biometrics in Improving Generic Stress Predictive Models. Journal of Sensors & Material, 1–12. http://arxiv.org/abs/1910.01770